Posted by: Clear Advantage in Featured, Uncategorized on June 28, 2023
Have you or someone you love recently found out you have keratoconus? Although it may sound scary, it doesn’t have to be.
Keratoconus is a progressive eye condition that affects the cornea. When you have keratoconus, the cornea becomes thin and bulges out into a cone-like shape.
Patients with keratoconus often suffer from visual distortion, light sensitivity, and difficulty completing daily tasks and activities. If you have keratoconus, understanding the condition and how to manage it is essential.
Keep reading to learn 8 things about keratoconus, including its causes, symptoms, and potential treatment options.
1. What is Keratoconus?
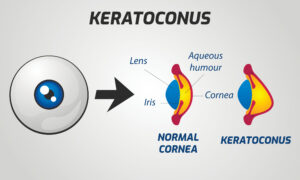
Keratoconus is a non-inflammatory eye condition that affects the shape of the cornea and the ability to see clearly. You may be more likely to develop keratoconus if you’re a teenager or in your early twenties.
When you have keratoconus, the cornea becomes too thin, making it more cone-shaped. The cornea should be round like you’d see with a baseball or basketball.
But with keratoconus, it’s closer to a football. The change in shape results in the cornea being less able to focus light onto the retina, making vision more distorted.
Patients with keratoconus may experience blurry vision or other frustrating symptoms.
2. Causes and Risk Factors of Keratoconus
Although the exact cause of keratoconus is not yet understood, certain factors are thought to contribute to its development. One of these is that keratoconus is hereditary and genetic, meaning you’re more likely to develop the eye condition if a member of your family has it.
There are also environmental factors like eye allergies, which may increase your risk of developing keratoconus if you rub your eyes a lot due to these allergies. Other health problems like asthma may also increase your risk of keratoconus.
If you think you may be at an increased risk of developing keratoconus, let your ophthalmologist know. With this information, they can monitor your eyes and vision for any signs of the eye condition.
3. Common Symptoms Associated with Keratoconus

Early detection is crucial when it comes to any eye condition, including keratoconus. Early detection means you can receive timely treatment and begin to manage the eye condition.
If you have the eye condition, you may experience symptoms like:
- Distorted or blurry vision
- Noticing more frequent changes to your glasses or contact lens prescription
- Becoming more sensitive to light
- Finding it more challenging to see at night
If these symptoms sound familiar, let your eye doctor know. The signs associated with keratoconus are not exclusive to this eye condition. Understanding the root cause of your symptoms will inform the best way to treat your eyes.
4. Diagnosing Keratoconus
If your eye doctor suspects you have keratoconus, the next step will be to schedule a comprehensive eye examination. During your comprehensive eye exam, your ophthalmologist will evaluate the shape and thickness of your cornea.
They will also measure your visual acuity and may use additional tests like corneal topography and pachymetry to confirm their diagnosis.
5. Does Keratoconus Progress?

Keratoconus is a progressive eye condition. It worsens over time.
Regular monitoring of the shape of the cornea and any changes to visual acuity are necessary to track how the eye condition is progressing. Having this information is needed for helping to monitor its progression and impact on your vision.
If necessary, your ophthalmologist will adjust treatment strategies.
6. How Do You Treat Keratoconus?
Several treatment options are available for managing keratoconus and improving your visual acuity. These include:
Glasses or Contact Lenses
During the early stages of keratoconus, you may be able to treat your vision using glasses or contact lenses. However, these will no longer be adequate as the eye condition progresses.
Other methods, like rigid gas permeable contact lenses or scleral contact lenses, might be a better option for improved visual outcomes.
Corneal Cross-Linking
Corneal cross-linking is a minimally invasive procedure that treats the early stages of keratoconus. It uses riboflavin eye drops applied to the cornea.
After applying these eye drops, the cornea is exposed to ultraviolet light. Corneal cross-linking helps strengthen corneal collagen fibers.
Doing this helps stabilize the cornea and slow down the progression of keratoconus. However, corneal cross-linking cannot reverse previous thinning of the cornea that has already occurred.
Intacs
In advanced cases of keratoconus, you may have tiny plastic inserts called Intacs surgically placed in the cornea. Using Intacs helps flatten the cornea and improve visual acuity in patients who no longer find using contact lenses helpful or effective.
Corneal Transplant
A corneal transplant may be considered for severe cases of keratoconus if other treatments have been insufficient. During a corneal transplant, the damaged cornea is replaced with a healthy cornea from a donor.
7. Living with Keratoconus

Keratoconus can significantly impact daily life, but patients can lead fulfilling lives with proper support and management. Joining support groups, maintaining regular eye examinations and appointments, protecting your eyes from excessive rubbing, and following the prescribed treatment plan can help manage the condition effectively.
Let your eye doctor know if a treatment is not working as expected.
8. Ongoing Research and Future Developments
Scientists and researchers continue to study keratoconus to better understand what causes the eye condition, why it progresses, and the best way to treat it. Exciting advancements like using laser technology with corneal cross-linking as potential future treatments for keratoconus patients are on the horizon.
Keratoconus is a progressive eye condition that requires early detection and proper management to preserve vision. By understanding the causes, symptoms, and available treatment options, patients diagnosed with keratoconus can work closely with their ophthalmologist to find the best treatment to manage the eye condition and continue living their life.
Regular eye exams and consistent follow-up care are essential for monitoring the condition’s progression and maintaining optimal visual health. Are you ready to conquer keratoconus?
Find out more by scheduling an appointment at Clear Advantage Vision Correction Center in Portsmouth, NH, now! Isn’t it time to take charge of your vision?